Grand Rounds, the weekly best of the medical blogosphere, is hosted this week at Code Blog. It’s a very readable and well-written edition, with some great posts as well. Grab a cup of coffee and and head on over!
Vitamin D Reduces Fractures
Vitamin D, if taken regularly and in doses higher than 400 IU daily, reduces fractures by up to 20% in older adults. So say researchers in a meta-analysis published in this month’s Archives on Internal Medicine.
Previous studies on the efficacy of vitamin D in preventing fractures have shown conflicting results, with some finding a benefits and others not. A team of Swiss and American researchers hypothesized that this variability in effect might be because some studies used too low a dose of Vitamin D and others did not accurately measure whether subjects even took the Vitamin D they were given. (We call that adnerence to therapy.) In addition, many previous studies did not control for baseline vitamin D levels or measure whether levels were actually increased with therapy.
In a complicated but nicely done meta-analysis, these researchers culled the cream of the crop of randomized clinical trails of vitamin D supplementation and fracture risk. Only studies that used higher doses of vitamin D, measured blood levels of Vitamin D and assessed subjects’ adherence to therapy were included in the analysis. The researchers compared fracture risk according to vitamin D dose and levels.
What they discovered was that doses of vitamin D of 400 IU daily were not effective in preventing fracture. Higher doses were – to the tune of a 20% reduction in non-vertebral fractures and an 18% reduction in vertebral fractures in individuals over age 65. (This is actually something that has been suspected for some time now, and in fact the current recommended daily dose of Vitamin D is 800 IU daily, with some saying that we should increase that further to 1200 IU daily.)
In support of the effect, fracture reduction was related to vitamin D levels, with higher levels showing greater reduction, up to a level of 112 nmol/ml (about 40 ng/ml). The benefits of vitamin D were seen irrespective of calcium supplementation.
The researchers recommend that future studies of Vitamin D and fracture risk use higher doses and longer duration of therapy, and measure both adherence to therapy and serum levels of vitamin D.
Take Home Message
Vitamin D indeed appears to be effective in reducing fracture risks, provided you adhere to your treatment and take over 400 IU daily. I’d recommend 800 IU daily. (And 1200 IU won’t hurt you…)
I’ve been measuring vitamin D levels in my patients with low bone mass, and have been not surprised to find that most of them are deficient. I love that I have an intervention for them that is both safe and inexpensive.
__________________________________________________
Prevention of Nonvertebral Fractures With Oral Vitamin D and Dose Dependency. A Meta-analysis of Randomized Controlled Trials. Heike A. Bischoff-Ferrari, DrPH; Walter C. Willett, DrPH; John B. Wong, MD; Andreas E. Stuck, MD; Hannes B. Staehelin, MD; E. John Orav, PhD; Anna Thoma, MD; Douglas P. Kiel, MD; Jana Henschkowski, MD. Arch Intern Med. 2009;169(6):551-561.
______________________________________________________
11/30/10 UPDATE
New IOM guidelines recommend vitamin D intake of 600 IU daily for adults up to age 70, and 800 IU daily for those age 71 and older.
Tickler Systems and Thoughts on Mandating the EMR
Dinosaur Doc posted awhile back about how she managed to keep track of a patient who was failing to follow through on a mammogram. Dino holds the charts of patients with pending studies on a special shelf in the file room, where they stay till the study comes back.
Dino’s got a tried and true tickler system, and it works.
My Old Paper Tickler System
I had a my own little tickler system before we went to an Electronic Medical Record. For labs and path, I had a cloth-bound log book, where my tech simply checked off the results as they came back each day before handing the pile of reports over to me for review. If the results didn’t come back, she called the lab. For radiology, we had a series of manila forders, one for each month of the year. When a radiology test was scheduled, the third NCR copy of the requisition was slipped into the pocket corresponding to the month in which the test was to be performed. As results came back, my secretary pulled the requisistions for the folder, and at the end of the month, anything left in the folder was overdue, and we contacted the patient. On my desk, I had a rack for the charts for patients who worried me or from whom I was waiting for call backs, and the chart stayed there until the issue was resolved or the game of phone tag was over.
My system was simple, it was fast and efficient, and it worked.
Tickling with the EMR
I’ve been electronic almost 3 years now, and have to admit, I still miss my old tickler system. What I’ve replaced it with is a bit more complicated. Here’s how it works (and anyone who has ideas on how I can do it better, please feel free to comment) –
Labs
This part’s easy. Most of my patients have labwork at our hospital, and the few who don’t go to Quest or Lab Corp, both of whom can send results electronically to our lab. I just head into my In Box to see their results. I go to the Overdue Results Folder once a week, sort it by type of test, and forward the overdue tests to my secretary. She then calls the lab or the patient (who occasionally skips out without their bloodwork).
If I am unable to reach a patient on the first try about an abnormal result in my In Box, I forward that result to myself as a Result Note, and those notes stay in a separate folder on the desktop till I hear back from the patient.
Rads
I handle radiology results in my In Box the same way as labs. But overdue rads are a whole ‘nuther story.
Today, after spending my entire Sunday cleaning up the Overdue Results Folder, I came up with an idea, and I can’t wait to try it tomorrow to see if it works. I’m going to order all my radiology as future orders, with an anticipated date around the time I expect it to be done. (I don’t know why I didn’t think of this before…) Of course, it’s now going to take me longer to place these orders, but I am hoping it will save me time at the back end and give me back a meaningful radiology tickler system.
Path
As for pathology, those reports come back quickly and pair nicely with their orders. But they lose their formatting when they come over from the path lab system to the EMR. Gone are the nice paragraphs separating the meat from the gravy, making it difficult to scan a report quickly to determine if it is normal or abnormal. As a result, I’ve actually missed a few abnormals since we went live with the EMR. Fortunately, our path lab still sends us a paper printout once a month of all our abnormal pap smears, and I caught my mistakes right away. Good old paper…..
Good Old Paper
Speaking of which, I find I still need a paper tickler system for those few patients I don’t want to lose track of. It’s quite a complex system – a lined paper pad that I keep on my desk. If I see a patient I am worried about, or get back a mammogram or abnormal pap that needs follow up testing, I write the patient’s name on the pad with a little box next to it. That box gets checked off when I get her colposcopy or breast biopsy results back, or whenever the issue at hand is resolved. I work through that list every 3-4 weeks or so, crossing things off and recopying the few remaining items to a new page in the pad to start all over again.
I wish our EMR would let me create my own folders for tracking my problem patients this way, but it does not. So I use paper.
I am not writing this post to whine or complain (Well, maybe a little…)
Our EMR is fantastic, and our programmers are top notch. As I sit in my bed at night reviewing labs or catching up on that day’s notes, or catch a medication interaction that I would have missed in the old days, I am forever grateful for the fact that my practice is electronic.
The problem remains, however, that we are still struggling to get our EMR optimized. It’s a patchwork created from different systems, each designed to do what they do well, but not necessarily all speaking the same language. As a clinician, I remain frustrated that we still can’t get them to talk fluently to one another. And that is why, in my humble opinion, we are not yet ready for mandated electronic medical records.
A Government-mandated EMR or Tower of Babel?
The current EMR did not just spring up anew one bright day. It has evolved over decades – decades in which the laboratories, radiology practices, hospital billing systems and some upstart clinical practices each took their operations to the computer, using propietary software systems developed specifically for their own niche. Dermatology and infertility practices each have online systems that were designed for the kinds of work flows unique to their business. Hospitals also have their own inpatient systems, which don’t necessarily translate easily into the physician office, and vice versa.
With all these separate systems out there, and more coming every day, I think we need to stop and take a deep breath before our national quest for an EMR becomes a government-mandated Tower of Babel. I don’t think any doc should be mandated to have an EMR until we have EMRs that can talk to one another. And our initial investment should not spending money on willy-nilly mandated installation of Walmart’s and other vendor’s systems, but on first developing a unified code and language to be used for all EMRs. Then we can see which of the currently used systems will fit into that paradigm, and spend our dollars tweaking existing systems or scrapping them for new ones that are up to code.
Perhaps we can take our cues from the banking systems. Those systems all talk to one another with a common language that has to work, or someone loses money. I don’t know how theses systems evolved, who set the standards or how they got universal agreement, but someone out there must know. Let’s get those guys onto our medical records task forces and see what they come up with.
Until then, I’ll be plowing through my Patchwork EMR Tickler system…
- Thanks to Chris Bandover for the Elmo Video
- Read more from TBTAM on Electronic Medical Records
Did You Know?
Okay, I’m probably very late to this party, but I just discovered this video (Thanks, Annette!) and had to share it in case any one else out there hasn’t seen it yet.
Did You Know? is based on a Powerpoint presentation called “Shift Happens”, created in 2006 for a faculty meeting by Karl Fisch, director of technology for Arapahoe High School outside of Denver –
I was hoping by telling some of these “stories” to our faculty, I could get them thinking about – and discussing with each other – the world our students are entering. To get them to really think about what our students are going to need to be successful in the 21st century, and then how that might impact what they do in their classrooms.
I believe in the transformative power of technology and its ability to empower individuals in ways that were unimaginable a mere decade ago. I believe that schools are approaching the point of dangerous irrelevance when it comes to preparing students adequately for their digital futures. The pace of change in schools is too slow and the pace of change in technology is too quick. I am a strong believer in public schools, but we need a new paradigm.
Refresh Your Grey’s Anatomy…
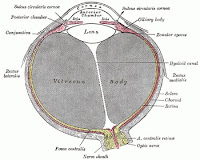 at the Sterile Eye, the blog of a Norwegian medical photographer, who hosts this week’s edition of Surgexperiences. For this edition of the best of the surgical blogosphere, the Sterile Eye puts down his camera, and takes us to a former age when the drawing reigned supreme…
at the Sterile Eye, the blog of a Norwegian medical photographer, who hosts this week’s edition of Surgexperiences. For this edition of the best of the surgical blogosphere, the Sterile Eye puts down his camera, and takes us to a former age when the drawing reigned supreme…
…nothing appeals to me like the simple and effective lithographs that accompanied the early editions of the tome of anatomical knowledge that is Gray’s Anatomy. The 1918 edition is in the public domain, and is available in its entirety online. All illustrations here, relating to the submitted posts, are taken from this edition.
Head on over for a compliation of surgical posts and some great illustrations.
Schlepperd’s Pie
Actually, the real name is Shepherd’s Pie, but we call it Schlepperd’s Pie, as in “Honey, I’m home from schlepping that herd of sheep back and forth over the same godforsaken mountain for the past 3 months. What’s for dinner?”
I’ve never actually made the Schlepperd’s – That’s Mr TBTAM’s job. He’s made it at least once a month for as long as we’ve been married, having learned how to make it from his Mom, whose husband was not a shepherd but a high school math teacher, which is almost the same thing.
Schlepperd’s Pie
The Brits make it with lamb. This is the American version with beef, sometimes called cottage pie, and is a very basic recipe. Other recipes call for carrots in the pie, but we like to serve our carrots on the side so we can spice them up a bit. (This dish itself is not exactly spicy, so we like to serve it with sides that carry a bit of punch.)
5-6 large Yukon Gold potatoes
4 tbsp butter
1 cup milk, more or less
2 tbsp vegetable oil
1 large or 2 medium onions, diced (not too small)
1 green pepper, diced (not too small)
1 1/2 – 2lbs ground beef
1 cup beef broth
1 tbsp flour
Paprika
Salt and pepper to taste
Peel and cut the potatoes into quarters. (If they are all different size potatoes, cut into pieces of roughly the same size, about 2 inches across.) Place in a large pot and cover with cold water. Add a pinch or two of salt and bring to a boil. Lower the heat to a low boil and cook until potatoes are tender. (About 20 mins.)
While the potatoes are cooking, preheat your oven to 350 degrees Fahrenheit. Then grab a big saute pan and heat up a the vegetable oil. Saute the onions and pepper over medium high heat till soft, about 5 minutes. Add the ground beef and saute till it just loses it color. Add flour and cook with the meat for a minute or so, then add the beef broth and stir in till slightly thickened, about 5 minutes or so. Season generously with salt and pepper and hold while you mash your potatoes.
Drain the potatoes. Add butter and milk and mash however you like. If you’re a purist, you can pass the potatoes through a food mill or potato ricer, heat up the milk and melt the butter before adding. If you’re like us, you’ll grab an electric mixer, toss in the butter whole and add the milk as you whip. (One of these days, I’m gonna get myself a potato ricer and see what all the fuss is about…) Season generously with salt and pepper.
Spread the beef mixture evenly across the bottom of a large ungreased baking dish (We use a La Creuset roaster pan). Spread the mashed potatoes evenly over the beef, careful to keep the layers separate. Sprinkle the top generously with paprika. Bake for 30 minutes, till the meat is bubbling and the potatoes are browned and gorgeous.
If you can, let the pie rest for about 10 minutes before serving.
________________________________________________________
We’re not the only ones who love Schlepperd’s Pie.
- Sass and Veracity makes a gorgeous pie with beef, lamb and pork
- A complex and interesting recipe from Tom Aikens at Food and Wine Magazine
- Shepherd’s pie talk at Chowhound
- Lamb and Eggplant Shepherd’s Pie at Chez Us
- The Moosewood Restaurant has a veggie version (of course)
- Spice O’Life makes a healthy version using ground turkey
- The Gluten-Free Goddess makes a spiced up versions that sounds delish
- Food Gawker makes it with sweet potatoes.
Jade Goody – Are There Lessons to be Learned?
No Margaret. You are confusing the UK with the USA. God knows, the NHS is creaking, and we have problems enough, but we do not have “public clinics” for the impoverished poor. In the USA, the impoverished poor, aka the unemployed working class, predominantly black and Latino, may need “public clinics”. In the UK everyone is entitled to a “primary physician” as of right, independent of status and means. Yes, yes, before someone, or no one, or “angry from Tonbridge” writes in, a few people slip through the net, and a few people have incompetent GPs, and there is a difficulty with the homeless who are of no fixed abode, and so on and so forth but by and large most people have a GP. God knows, I do not hold back on criticising the failings of the NHS, but I become amazingly protective when people try to suggest that we have problems akin to those experienced by the medically uninsured in the USA.
I encourage you to head on over and read his post, which includes a description of the cervical cancer screening program in the UK.
Dr Crippen also thinks I went too far in hoping that someone
personally called, warned, cajoled and hollered at [Jade] countless times, until finally, as a last ditch effort, they sent her a certified letter.
You know what? He’s right. I doubt I would have called “countless times”. I was being a bit hyperbolic, probably because I was feeling particularly saddened and frustrated by the fact that a preventable death was about to occur in a young mother of two children.
But I like to think that I would have called Jade at least once if she failed to respond to her letter. Probably twice if I know myself well. And I suspect from reading Dr Crippen’s post that he would have done the same.
So don’t worry, Dr Crippen – you and I are in full agreement that the medical profession does not need anyone breathing down our backs to force patients to accept medical care that they have been duly informed that they need. I was in no way trying to insinuate that the medical profession bore any legal responsibility in Jade’s tragedy. They sent her a letter, she ignored it. Her bad.
That said, the question that remains is simply this – Did anyone call Jade when she failed to follow up on that last abnormal pap smear?
Which is not to imply that they were required to do so, or that the government should mandate it. I’m just speaking as one human being to another. It seems like it would have been the right thing to do.
And I hope someone did it.
That was really all I meant to say.
Pregnancy – Week by Week or Pound by Pound?
The essay made me so sad.
It is the typical story of the modern woman’s experience of her body during pregnancy. A journey that begins with joy but quickly turns to self-loathing and sadness –
Almost from the moment I found out I was pregnant, I felt hugely fat…. When I finally had to accept, at the end of month four, that I was now a whole dress size bigger, I actually cried – and went out to buy a pair of size 12 jeans.
This is a woman carrying her first child, and instead of joy, she feels – fat. It’s just wrong. (And yet who among us has not felt the same way?…)
Fortunately, by her fifth month, Smith begins to enjoy her pregnant body.
Bizarrely, though, I suddenly felt hugely confident….I even started to get a thrill from seeing the needle on the scales inching its way towards the 131/2 stone where it would end up… Friends would say reassuringly that most of that extra weight was the baby, and I actually felt rather gleeful as I replied that, no, the baby inside me weighed just a few pounds – and any extra weight was in fact me.
Well, Ms Smith, I think I need to correct you there. Technically, yes, much of the added weight was you. But much more than a few pounds was related to the baby.
Don’t believe me? Here’s how it breaks down in a normal singleton pregnancy –
Weight Gain in Pregnancy
- Baby – 7.5 lbs (more or less)
- Placenta – 1.4 lbs
- Amniotic fluid – 2 lbs
- Increase in uterine weight – 2 lbs
- Increase in breasts – 2 lb (more for some)
- Increase in blood volume – 3 lbs
- Increase in extracellular fluid (no edema ) 4 lbs
That’s over 20 lbs right there without a single ounce of extra fat gained. Most women will gain about 7 pounds of adipose during pregnancy, for a total normal weight gain of about 30 pounds. But I’d give Natasha another 5 lbs or so for those swollen ankles in her last few weeks.
Now, Smith did gain a bit more than 30 pounds.
She went from about 130 lbs to 188 lbs, for a total gain of 58 pounds. And yet, by 5 months post partum, she’s dropped all but 14 pounds of her pregnancy weight!
I’d say she’s doing just fine. Once she starts to sleep a bit more through the night, it’ll all be gone.
Why do I say that? Well, studies have shown that mom’s weight at one year postparum is inversely related to how many hours her baby is sleeping through the night at 6 months of age. Given that Smith still has a few extra pounds on her, I’d wager little Finn is still up for nightime feeds.
Bottom Line
Our obsession with weight is ruining our experience of our own pregnancies, whittling away little pieces of joy during one of the most special times of our lives.
Instead of worrying about our weight while we are pregnant, we should be finding ways to help new moms get the sleep they need.
_________________________________________________
Photo by Caroline Marks at The Daily Mail online
Multimedia Grand Rounds at Doc Gurley
 An amazing grand rounds is up this week at Doc Guley’s site. There a webcast, including conversations with many of your favorite medical bloggers, viewer polls and great jokes such as this-
An amazing grand rounds is up this week at Doc Guley’s site. There a webcast, including conversations with many of your favorite medical bloggers, viewer polls and great jokes such as this- Nurse: Doctor, there’s an invisible man in the waiting room.Doctor : I’m too busy – tell him I can’t see him
Doc Guley – You may have topped your famous Lost Tampon Video.
Head on over for a listen and a look at this week’s best of the medical blogosphere.
The Invention of the Sims Speculum – Surgical Improvisation
This post was inspired by Doc Gurley’s call for submissions to this week’s Grand Rounds, the theme of which is Improvisation.
Sims was a family doctor practicing in Montgomery, Alabama in the mid 1800’s. Although he had no expertise in or desire to treat “women’s disorders”, he was referred, in quick succession, three young African slaves suffering from vesicovaginal fistula – a hole between the vagina and the bladder that develops as a result of prolonged obstructed labor. No one had yet developed an operation that could cure the condition, and Sims had declared the women inoperable.
But just before he was about to send the third young women back to her owner’s plantation to live forever with her debilitating condition, something happened that changed both Sim’s mind and the field of medicine forever.
Sims was called upon to care emergently for a white woman who fell from her horse and who was in great pelvic pain. Assuming that her pain was from acute malposition of the uterus, and remembering a trick taught to him by one of his former professors, Sims asked the woman to get on her knees and elbows. He then inserted two fingers into the vagina, vigorously pumping up and down to reposition the uterus. As he did this, the woman’s uterus fell back into position, relieving her pain. At that moment, a large amount of air burst from the vagina. Although this embarrassed the woman, it gave Sims an idea of how he might help the African slave languishing untreated in his backyard hospital.
If depressing the vaginal walls allowed air to get into the vaginal cavity, could he somehow create an instrument to do the same thing and allow access to the area of the fistula?
Forgetting everything for the moment except the value of this important revelation he jumped into his buggy and drove hurriedly to a hardware store in Montgomery where he bought a set of pewter spoons of different sizes. Bending the bowl and part of the handle of one of these at a right angle he placed one of his patients suffering from vesico vaginal fistula in the genupectoral position, inserted the improvised speculum and atmospheric pressure accomplished the rest. The fistulous opening was clearly seen.
“Introducing the bent handle of the spoon I saw everything as no man had ever seen before. The fistula was as plain as the nose on a man’s face. The edges were clear and well defined and the opening could be measured as accurately as if it had been cut out of a piece of plain paper. The walls of the vagina could be seen closing in every direction. The neck of the uterus was distinct and well defined and even the secretions from the neck could be seen as a tear glistening in the eye clear even and distinct and as plain as could be. I said at once “Why can not these things be cured?”
Sims operated using his speculum, but the operation failed. The fistula persisted, albeit smaller than before. It would be years, and many more operations on these same women and others, before he perfected a surgical technique using silver wire suture that resolved the fistulae completely.
 Over time, Sims would come under increasing scrutiny and criticism for what some said was unethical experimentation on his patients, who were all female slaves, and whose operations were performed without anesthesia. Sims did give post operative pain relief, in the form of large amounts of opium – another practice that put him under suspicion.
Over time, Sims would come under increasing scrutiny and criticism for what some said was unethical experimentation on his patients, who were all female slaves, and whose operations were performed without anesthesia. Sims did give post operative pain relief, in the form of large amounts of opium – another practice that put him under suspicion. Reportedly, Sim’s patients themselves remained faithful to him in their desperate hope to resolve their plight – faithful to the point of serving as his surgical assistants when his medical colleagues abandoned him to his experiments.
Some say Sims used the African slaves to experiment on surgical techniques he would someday use with white women under anesthesia, and condemn Sims as a racist monster. Others say he was just a man of his time who gave away service for free to slaves suffering from what had been heretofore an incurable condition.
Whatever you think of Sims, it is important that we remember and honor the three slave women who served as his patients, and known only by their first names – Anarcha, Lucy and Betsey.
It is also important to remember that even today, over two million women in sub-Saharan Africa and Asia suffer from vaginal fistula, as a result of unattended childbirth and violent rape. International efforts are being directed at treatment for these women, but prevention demands that all women have access to skilled birth attendance and access to emergency obstetrical care.
____________________________________________________
Sources –
Sims, JM. The Story of My Life. New York, D Appleton & Co, 1894. via Google Books.
Harris, Seale, MD. Women’s Surgeon – The Life Story of Marion Sims. New York, The MacMillan Company, 1950.
Sartin, JS. J Marion Sims, the Father of Gynecology – Hero or Villain?
Ojunaga, D. The Medical Ethics of the Father of Gynecology“. Journal of Medical Ethics 1993; 19: 28-31.
Sims Speculum image from Wikipedia. Surgery Image from National Library of Medicine.
Brain Twister
The good news is that I get to perform this hilarious monologue based on Thomas Meehan’s “Yma Dream” in my musical theater class production of “The No Frills Revue“.
The bad news is that I have to memorize it.
Grand Rounds at Health Business Blog
David Williams hosts this week’s edition of the best of the medical blogosphere. It’s a great edition. Topics covered include –
- The Octuplet’s IVF doctor – Take away his license, says Toni Brayer. I say California taxpayers should sue him for the cost of raising that family he created.
- The Entepreneurial MD where the money is for docs in Obama’s stimulus package. ( Dr Wes can tell you the researchers are lining up for the bucks…)
- How to win over docs to evidence -based medicine – Get them Up to Date, says Dr Val. I agree.
The Other Mediterranean Diet- Chickpea Salad
With all this talk about the Mediterranean Diet, I think we sometimes forget to look beyond Greece, Spain and Italy for delicious and healthy foods. I’m speaking of course, of the wonderfully healthy and fascinating cuisines of the Middle East.
This weekend I discovered a most wonderful Middle Eastern cookbook – The Arab Table by May S. Bsisu. The book is a culinary tour of the Arabian countries of the Middle East – Palestine, Jordan, Yemen, Syria, Morocco, Syria, Egypt and the Arabian Gulf – along with family reminiscences and explanations of customs and holidays that give cultural context to every recipe.
If this, our first foray into May Bsisu’s recipes is any prediction, I’d say the Arab Table is going to become a source of meal ideas at our table for a long time to come.
Dressed Chickpeas
The strong saltiness, cumin and cayenne flavors in this dish may be an acquired taste for some, so I recommend using a third to half the amounts listed below to start and adjusting upwards if you like the flavors. (I happen to love them.) I love parsley, so I actually used almost a 1/4 cup in mine. Bsisu tells us to add feta to turn this side dish into a satisfying lunch. If you do that, I’d serve it on a plate atop a bed of lettuce leaves.
2 cans chickpeas
1 jalapeno pepper, seeded and minced
1/2 pound white onions, finely chopped
2 cloves garlic, mashed
1 1/2 tsp kosher salt
1 1/2 tsp ground cumin
1/4 cup fresh lemon juice
1/3 cup extra virgin olive oil
1 medium tomato, chopped, for garnish
1 tbsp coarsely chopped fresh parsley, for garnish
1/2 tsp cayenne pepper, for garnish
Drain chickpeas and rinse three times under running water. Place in saucepan with water to cover 1 inch, bring to a boil and cook for 1-2 minutes. Drain and cool a few minutes in the colander, then place into a large bowl of cold water. Gently rub the chickpeas between your palms to remove the skins until most of the skins are removed, replenishing the water once or twice as it becomes covered with the skins.
Place the drained chickpeas in a large bowl and add the onion and jalapeno.
Whisk the garlic, salt, cumin, lemon juice and olive oil together in a small bowl. Pour the dressing over the chickpea mixture and toss gently. Serve on a bed of lettuce leaves garnished with tomatoes and parsley.
________________________________________
Map from Wikipedia
The Tragedy of Jade Goody
 Jade Goody, the controversial star of British reality TV, is dying of cervical cancer at age 27. This young woman, who has lived her life in front of the camera for the last 7 years, will die for the camera as well, having sold the rights to film her last days in an ongoing reality show.
Jade Goody, the controversial star of British reality TV, is dying of cervical cancer at age 27. This young woman, who has lived her life in front of the camera for the last 7 years, will die for the camera as well, having sold the rights to film her last days in an ongoing reality show.
Whatever you think of Jade, the publicity generated by her illness has led to a 20% upswing in the number of women getting Pap smears in Britain.
And this is a good thing. Because if Jade’s story causes even one young woman to get the smear that saves her life, it will mean Jade’s death will not have been in vain.
The Irony
Unlike Eva Peron, whose death from cervical cancer occurred in the years before we had access to screening, Jade did get pap smears.
Jade had more than one pap smear, starting in her teens. At one point, she was even treated for precancerous changes of the cervix. And went on to have more follow up smears after that.
But when those follow up smears showed a recurrence of abnormal cells, Jade ignored letters that were sent to her advising her to come in for follow up and treatment.
Why? Because she was scared..
“They had sent a letter to me ages ago, telling that I needed to go in for an operation, but I had been too scared to do anything about it,” Goody confessed.
So Jade put the whole thing out of her mind and pretended it never happened. Until repeated episodes of pain and hemorrhage became symptoms she could no longer ignore. But by then, the tumor had spread beyond the cervix to her uterus. And while a radical hysterectomy and chemotherapy staved the cancer off for awhile, it returned this past month with a vengeance.
And now Jane Goody is going to die.
Let me stop beating around the bush
What has been on my mind all week since I first read about Jade’s story, and what I want to ask is simply this –
Did any health professional ever actually call Jade and try to get her in for treatment in all that time after her Paps came back abnormal? A nurse? A doctor? Anyone?
Please don’t tell me the only contact ever made with this frightened young woman was a series of letters, each one scarier than the next. Please tell me someone called her personally and tried to get her in.
Look, I know Jade was stupid.
No one, even Jade, I suspect, would say otherwise. Ignoring multiple abnormal Pap smear letters was not the first or the last stupid thing Jade Goody ever did. This is a kid who, in front of millions, stripped nude during a game of poker, made an ass of herself shouting racial slurs to an Indian housemate and then gave a blow job under the covers to another housemate. We’re not talking rocket scientist here.
But I’ve seen Jade in interviews that I’ve watched over the past few days, trying to wrap my head around this tragedy. This kid doesn’t hold anything back. She is completely genuine, self-effacing and ready to admit her shortcomings. She’s an idiot, but she knows it. And she is anything but unreachable emotionally. I just can’t believe that someone couldn’t have convinced her to come in sooner if they’d just talked to her.
Please tell me someone tried to reach her.
Jade seems to have had multiple interactions with the health care system during those years between the abnormal smears and her ultimate diagnosis. Times when she visited doctors for pain or gastrointestinal symptoms that were probably related to her growing cancer.
Did these doctors know about her abnormal smears? Did Jade think to tell them? (Probably not…) Were the letters being sent from the NHS cervical cancer screening program separate from Jade’s actual ongoing medical care?
Heck, did Jade even have a source of ongoing care, or, god forbid, a primary physician? I doubt it. This is, after all, a lower class girl from a very rough upbringing – someone, I suspect, whose only contact with the health care system was in public clinics and ERs. She probably bounced around ER’s and hospitals during those years, failing follow up appointments, checking out AMA so she could appear in one or another publicity venue, denying that there was really anything wrong. (Update – Dr Crippen corrects my misperceptions of the British system…)
She even tried to delay her surgery after her diagnosis so she could stay on TV, till they told her she’d be dead in 3 weeks unless she went into the hospital right away.
So maybe I’m completely off base.
Maybe, just maybe, there were docs and nurses who tried to help Jade. Folks who personally called, warned, cajoled and hollered at her countless times, until finally, as a last ditch effort, they sent her a certified letter. Health professional who really cared about Jade and wanted to help her, although ultimately she refused their help.
Maybe Jade was just really that stupid.
I hope so. Because otherwise, the tragedy is not just Jade’s, but all of ours.
______________________________________________________
Update –
Dr Crippen reponds to my post with a very thoughtful post of his own regarding Jade.
I respond to Dr Crippen.
For more information about cervical cancer, see these sites –
Jade Goody Photo from Wikimedia
Healthcare Hedging
I saw a patient this morning for an emergency appointment.
The emergency? Her husband is suddenly losing his job due to downsizing at his firm, which is losing contracts in the bad economy. She wanted to get her annual appointment in before March 1, when his insurance coverage ends. (She is a self-employed minister and they have no other insurance.)
Her exam was fine. We got her squeezed in for a mammogram and a bone density tomorrow. (She has had osteopenia and has been on a bisphosphonate for a number of years.)
But here was my dilemma – If her bone density is not improved, I would want to check a vitamin D level and urine NTX. If it is improving, I probably would not do these tests this year.
But by the time I get the results of her bone density, her insurance will have run out and she won’t be able to afford the tests.
So I did the tests today, even though I don’t know yet if I will need the results to manage her condition. She is also refilling her bisphosphonate for another 90 day supply, even though there is a chance I will discontinue it if her bone density is improved significantly.
Of course, their COBRA could end up coming through, in which case we could have waited and potentially saved the system the cost of those test and her meds. But she won’t hear about that coverage till next week.
She also asked if, while I was at it, I could send off “a panel of tests” that she might need in the upcoming year, but that I refused to do. She just saw her rheumatologist 6 months ago, after all.
And I can only potentially waste so much of the American healthcare dollar.



